

We created a run chart showing the frequency of the prone position by week. Patients who were maximal assist typically took longer periods of time to reposition and usually did not tolerate the prone position well. The expanding population of patients with COVID-19 led to the development of triage criteria for our prone positioning team to focus on patients who required moderate assist rather than maximal assist. Pharmacologic interventions for sleep or anxiety were also proposed in select cases. Anxiety (especially for patients who couldn’t return to an upright position on their own due to decreased mobility) was addressed by placing devices such as phones and call buttons within reach.Coughing fits and transient hypoxia were addressed by using a stepwise process of prone positioning.We also included fields on nursing flowsheets in the electronic medical record to indicate patient position.ĭuring the course of this initiative, challenges and barriers arose, and modifications were made to address emerging challenges and barriers, including: We developed note templates for prone positioning for the physical therapist prone positioning team. Our physical therapist-run team promoted prone positioning by assisting patients who were less mobile into the prone position – optimizing for safety and comfort.Ĥ. To our knowledge, our effort represents the first instance of a prone positioning team for awake patients, although prone positioning teams have been described in patients intubated in the ICU setting. Led by a wound, ostomy and continence nursing team, we sought appropriate supplies to maximize comfort and reduce pressure injuries in the supply-limited setting of the pandemic peak.ģ. Optimization of supply management and operations.
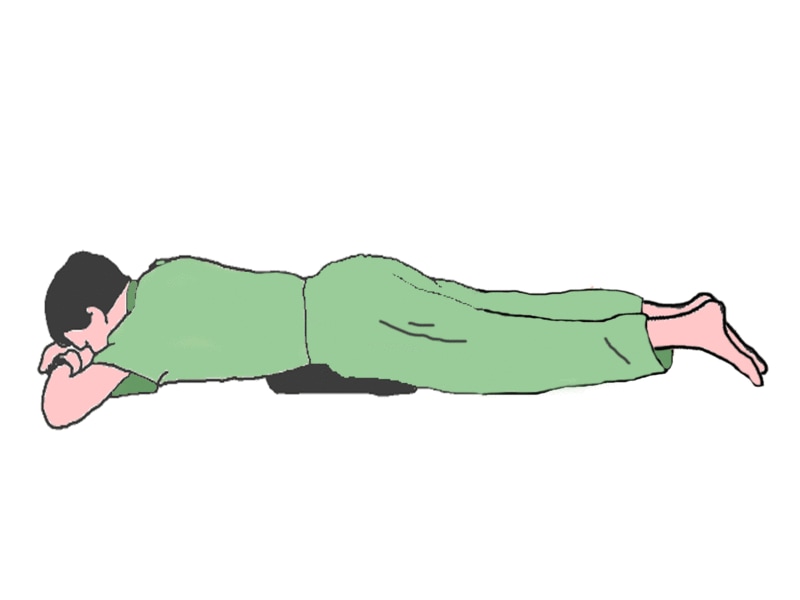
precautions to insure comfort and safetyĢ.This included a ‘one-pager’ handout with information for patients and nurses, as well as an instructional in-service video. Nursing, physical therapy, physician and patient education. Our initiative, detailed in the article, “Increasing Rates of Prone Positioning in Acute Care Patients with COVID-19,” from the January 2022 issue of The Joint Commission Journal on Quality and Patient Safety, consisted of four separate interventions:ġ. While efforts were underway to develop prone positioning teams for intubated patients, we launched a multidisciplinary initiative to increase prone positioning among patients with respiratory failure, but who did not yet need intubation or ICU level care. All these are especially true in older and less mobile patients, who may stand the most to gain from prone positioning. It also can be interrupted by meals or other clinical interventions undertaken during the course of a hospitalization. Some might be too weak to turn over on their own. It can put some at risk for pressure injuries. 2įor many patients, the position is uncomfortable or painful. Evidence suggests prone positioning must be sustained for some time for it to have an effect. Getting large numbers of people into the prone position is limited by patient and operational barriers.
:max_bytes(150000):strip_icc()/positions-5bb0f1d74cedfd002615d0ca.png)
1 During the initial wave of COVID-19, prone positioning in non-intubated patients outside the ICU was proposed as a safe way to help prevent progression to intubation and death. Placing patients on their stomach, known as ‘prone positioning,’ has been demonstrated as a successful intervention to improve outcomes in patients intubated with acute respiratory distress syndrome.


 0 kommentar(er)
0 kommentar(er)
